By Howard Mavity
I remember the near hysteria and the lack of clear workplace and public health guidance when I began receiving questions about responding to AIDS in the workplace in 1984. If you have forgotten how people reacted, watch the excellent Dallas Buyers Club.
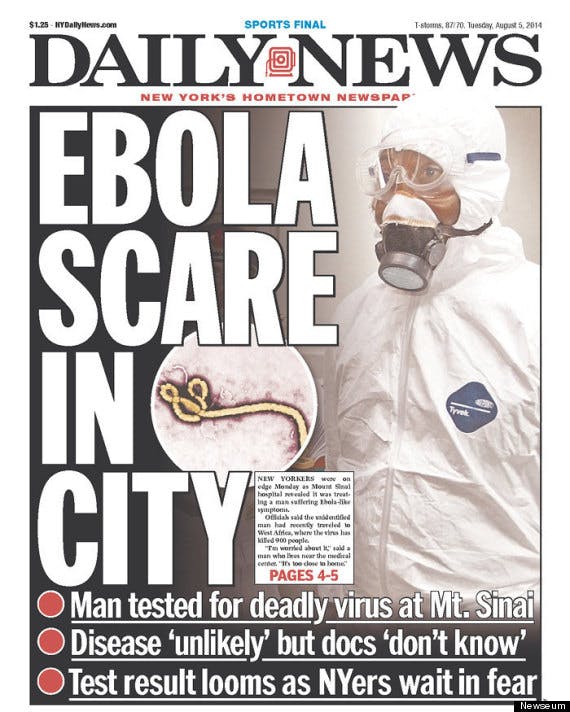
We’re in a similar situation with Ebola.
We don’t yet know enough about the transmission and prevention of Ebola to develop the detailed black-and-white procedures that give us a real or imagined sense of security. And even more than HIV, Ebola is a graphically frightening disease. The fatality rate is high, the death is swift, and the presentation is horrific.
Lessons from AIDS in the 80’s and 90’s
But let’s step back, and consider what we learned with AIDS.
HIV was less easily transmitted than first believed. Rash decisions about HIV positive employees got one sued under the Americans with Disabilities Act (ADA) or other legal scheme. The disease also triggered advances in medical precautions such as the OSHA Bloodborne Pathogens Standard, Needle Stick rules and more sophisticated Personal Protective Equipment (PPE).
Thirty years later, instead of panicking, co-workers tend to pull together and support a co-worker who is HIV positive.
Application to Ebola
As with AIDS in the 80’s, we simply do not yet know enough about the disease. We’re at the midpoint in our learning curve (read the book The Hot Zone and you’ll see that we’re not quite as ignorant about Ebola as one might think). However, unlike HIV, Ebola appears to be more easily transmitted.
We learned that HIV was transmitted through certain specific activities. As one CDC commentator said in the early 90s, “you may get AIDS sitting on a toilet, but only if you’re having sex while doing so.” I’m not being flippant. The HIV virus is not especially hardy.
Ebola, on the other hand, initially appears to be more readily transferred through contact with bodily materials. Public Health Authorities continue to believe that true airborne transmission does not occur, but questions remain about the extent to which sneezes or other expulsions of bodily fluid can transmit the disease. (See the CDC Fact Sheet on Transmission of Ebola).
This weekend’s announcement of a second Dallas health care worker testing positive raised the public’s anxiety level, because the nurse claims to have followed proper protocol. I suspect that the worker must have inadvertently exposed herself to infectious materials while removing gloves, gown and face shield.
However, how significant was the exposure? Did the employee encounter material when taking off PPE? Touch her face or mouth? We don’t yet know.
Surely we are not faced with a need for laboratory level decontamination. Most employers are not equipped for that level of protection, and current staffing arrangements would not permit this approach if Ebola was widespread in the U.S. (See the CDC Guidance on using PPE)
Take a deep breath
So you can see why both lay people and healthcare professionals will be anxious until such questions are answered. But let’s consider why Ebola should perhaps worry us less than HIV.
So far, the U.S. has been successful in limiting the disease from crossing our borders. It was impossible to prevent HIV-positive individuals from entering the U.S., and to put it bluntly, would we have really wanted to do so?
Terrifying though Ebola is, the disease so far is limited to a small number of lightly populated nations with limited travel to and dealings with the rest of the world. (See the CDC List). Also, Nigeria, as well as certain West African nations, such as Uganda and Kenya appear to be on the top of the concern.
I do not know if the current airport screening is adequate or if more restrictions are needed, but the truth is that a country like the U.S. has the infrastructure, culture and health care system to limit Ebola’s entry and spread. Far more problematic is what the world must do about East Africa. I do not believe that the world can realistically isolate and leave these nations to become a hellish breeding ground for even more dangerous mutations, but that’s not my responsibility.
Step 1 – Stay alert and do not make rash decisions
We have learned from HIV, hepatitis, and the various pandemics that the law tracks and relies upon CDC and other public health guidance.
As best you can, try to apply and follow this guidance in your risk management. Monitor and keep up with developments. Be suspicious of what you read in the news.
School setting
Next to the health care workplace, schools are the most sensitive and emotional area. Until the guidance changes, we don’t need to treat every world traveler or even every African traveler as an Ebola risk.
Schools and employers must do some fact-finding. Are they from an affected country or from a neighboring country or one who has gained control of Ebola within their borders? Your response will vary depending upon the answers to these questions.
Belt and suspender approach?
Let’s use the school setting for analysis. The risks and the public concerns are great. You saw the frenzy in Dallas following the death of the man who came to the U.S. to see his family. Follow the CDC guidance, and administration may choose to follow additional “reasonable” precautions depending on the situation.
A school may decide to require the returning student to again undergo the very basic screening currently being carried out in U.S. airports. (See the CDC Handout.) Early on, the illness presents like many other diseases, so fever seems to be the main trigger depending on the person’s background. (See the CDC symptoms list.)
Depending on the facts and the risk tolerance, the organization may choose to do more. However, be thoughtful and do not make knee-jerk decisions. Ebola is certainly a real or perceived disability condition under the ADA, and other state and federal laws are also implicated.
Communicating with employees and family
We don’t have space for a full ADA tutorial, but so long as it is work-related and objectively reasonable, you may need to ask workers, students or members of the public, the same sort of questions referenced in CDC guidance to determine possible exposure to or development of Ebola. (See the CDC Page).
But, do so thoughtfully and in compliance with CDC guidance. Ask yourself, “how will this later look to a government agency or court?” Examples: CDC Ebola page; CDC Health Care Setting Guidance.
Worker safety
We are concerned with more than health care settings. Workers at JFK Airport involved in cleaning and servicing aircraft carried out a symbolic one-day strike last week over concerns about exposure within aircraft. The SEIU, sensing an opportunity to sign up employees in their union, provided “classes” on proper use of PPE and work practices when cleaning or working in aircrafts.
From Reuters:
About 200 airline cabin cleaners walked off the job at New York’s LaGuardia Airport on Thursday to protest what they say is insufficient protection from exposure to Ebola for workers whose jobs include cleaning up vomit and bathrooms.
Picket lines were set up overnight by non-unionized Air Serv cleaners outside Terminal D at LaGuardia for a one-day strike prompted by fears about the deadly virus, forcing airline crews to clean the planes themselves. Some signs read “Air Serv exposes us to vomit, blood and feces without protection” and “Air Serv puts worker safety at risk.”
The workers, who are trying to join Service Employees International Union, the largest service workers union in the United States, briefly left the strike line to attend an infectious disease training session organized by the union.
The minimal training lasted less than an hour and focused on removing contaminated gloves and washing up properly after potential exposure.
It was attended by workers from LaGuardia and John F. Kennedy International Airport, who fumbled with putting on and taking off bright blue and green latex gloves, which they said were thicker and better quality than the ones supplied by their employer.
There are OSHA and consensus standards implicated by duties such as cleaning aircraft. We have already encountered Bloodborne Pathogens Programs, Needle stick and Hazard Communication issues in cleaning aircraft. (See the OSHA Ebola page).
Follow the logical entry points and you can see other types of workplaces which may be exposed in the transportation industry. But there will also be overreaction and unneeded angst.
Workers complaints and refusal to work
Here are some basic considerations:
- Under Federal and State-OSHA whistleblower protection, an employee may not take adverse action against your employee for making safety complaints, even if the complaints are unreasonable.
- Under OSHA anti-retaliation provisions, there is a more demanding standing for refusing to work, and normally the employer’s safety concerns must be reasonable.
- The NLRB will likely treat many employee refusals to work because of safety concerns as “protected concerned activity.”
Sharing information
It behooves employers to immediately (as in now!) get out front and update employees about Ebola and why they should or shouldn’t be concerned.
Use the opportunity to remind employees about the Flu Season, the value of Flu shots, and the absolute need for hand washing. Try to prevent hysterical reactions by educating employees before a real or perceived incident occurs.
As in the case of HIV, Hep-b, TB, and other infectious diseases, the ADA and common law privacy laws strictly limits when and how an employer may share individual employee information. Generally, once one develops the facts, there is no meaningful risk, and once employees understand the lack of risk, one can calm the situation.
As we have learned when an employee presents active TB, there are occasions when more information may be shared, and proper ways to do so.
Stay tuned for more information.
This was originally published on Fisher & Phillips’ Workplace Safety and Health Law Blog.